Peripheral Artery Disease (PAD)
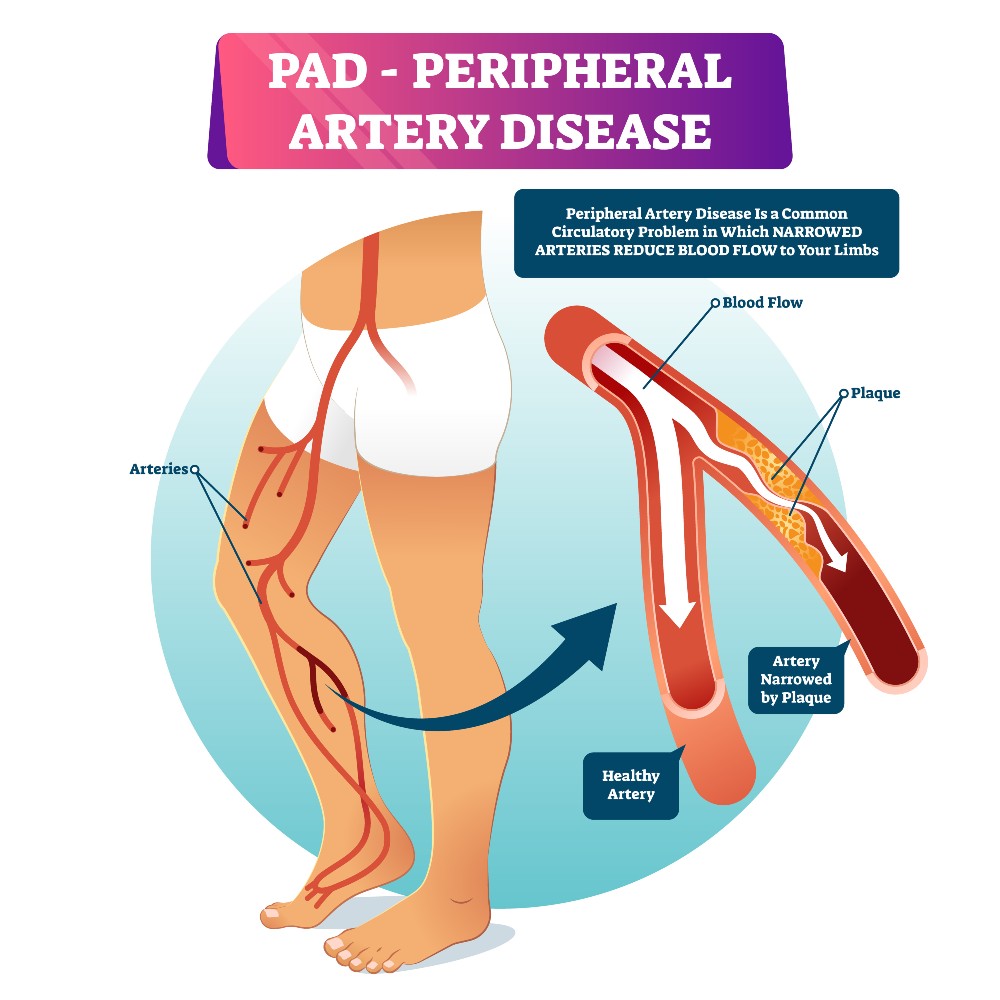
Peripheral Artery Disease (PAD) is a cardiovascular disease that affects the blood vessels. It occurs when fatty plaque builds up in the vessels, making it difficult for oxygen-rich blood to be dispersed across the body, especially to the lower extremities. According to the Centers for Disease Control and Prevention, approximately 6.5 million people, age 40 and older in the United States have been diagnosed with PAD. While PAD can occur within any blood vessel, the disease tends to form in the legs.
PAD’s most severe and advanced stage involves the development of critical limb ischemia (CLI), a dangerous condition that involves blood vessels within the legs becoming so severely blocked that tissue damage results, and amputation may be necessary. PAD also increases your risk of suffering a heart attack or stroke.
It’s important to know that PAD is a preventable disease. If you or someone you know suspects that they have PAD, receiving treatment sooner rather than later can, according to American Heart Association, slow the disease’s progression and even reverse symptoms.
What Are the Symptoms of PAD?
Symptoms of PAD include leg pain, cramping, tingling, weakness, and/or achiness. Many people with PAD report that their legs hurt after performing physical activity (such as walking), but the pain subsides when the body is at rest. It’s possible, however, for some people with PAD to have no leg pain at all.
Visible symptoms of PAD include hair loss; decreased or absent pulses in the feet; skin that appears smooth and shiny; muscle atrophy; skin discoloration; sores or ulcers in the lower extremities that aren’t healing properly; cold or numb toes; brittle and slow-growing toenails; and skin that is cool to the touch.
How Can I Prevent PAD?
There are ways to prevent PAD. If you smoke, quit; tobacco use not only significantly increases your chance of developing PAD, but also makes symptoms of the disease worse.
If you have high blood pressure or high cholesterol, see your doctor to get these issues under control. Also, try to follow a diet low in trans and saturated fats, which can help lower cholesterol levels.
If you have diabetes, talk to your doctor about managing your diabetes effectively.
It’s also important to stay fit and active. Aim to go for a 30-minute walk at least 3 to 5 times per week. The Vascular Disease Foundation states, “Recent studies show that for many people with PAD, a structured walking program is one of the best treatments for reducing leg pain or cramps (claudication) when walking. Studies show that over time a structured walking program is often more effective and can work better than medicine or surgery in helping people with PAD walk longer and further without having to stop due to pain.”
In addition, if your primary doctor has prescribed medication for cholesterol, high blood pressure, anti-coagulants, or another medical issue, be sure to take your medication as prescribed.
Visiting your doctor regularly is also an excellent way to prevent PAD.
What Causes PAD?
PAD is caused by blocked or clogged arteries. Over time, the arteries have filled with fatty plaque, which inhibits blood flow. When blood flow is inhibited, especially in the lower extremities, it’s difficult for blood to reach tissues in the legs and supply those tissues with sufficient oxygen and nutrients.
How to Test for PAD
Your doctor can perform all the tests necessary to determine if you have PAD. Those tests may include but are not limited to bloodwork, a doppler ultrasound, and imaging tests.
Smart ABI
A new tool called Smart ABI is a crucial part of PAD testing. It’s a reliable way and non-intrusive way for your doctors to determine if you have PAD.
Smart Ankle Brachial Index (or Smart ABI) involves testing your circulation by focusing on two crucial measurements: blood pressure and ABI. Using Bluetooth technology, the Smart ABI allows our doctor to accurately measure the blood pressure in your ankle and the blood pressure in your arm. During this painless and straightforward test, you will be fitted with a comfortable cuff. The first measurements are taken at rest, and the second after a walking exercise.
Once the numbers of the two pressures are revealed and carefully compared, our doctor can make a confident diagnosis. Lower figures indicate that the arteries are narrowed or blocked. If you are diagnosed with PAD, our doctor will discuss the appropriate treatments.
Treatments for PAD
If you’re diagnosed with PAD, our doctor will discuss your specific treatment options. Some patients are prescribed antiplatelet medicines, which are meant to prevent serious complications that may arise.
Our doctor may recommend a supervised PAD walking program.
In some cases, surgery—including angioplasty or an artery bypass graft—may be required.
Our doctor will be able to provide the most insight into the severity of your PAD and will recommend the best treatment options available to you.
Contact Us for Getting Tested for PAD!
When it comes to PAD, early detection is essential.
Here at Burlington County Foot & Ankle Associates, Inc., we are pleased to inform our patients that we use Smart ABI to test for PAD. Dr. John Palma is well-versed in PAD and other circulatory conditions that can affect your legs and feet.
If you are concerned that you may have PAD, please contact us as soon as possible by calling 609-714-0052 or by filling out the convenient contact form on our website. Burlington County Foot & Ankle Associates, Inc. is here to help by giving you the answers you seek and the thorough evaluation you deserve.
FILL OUT THE FORM TO
CONTACT US
© Burlington County Foot & Ankle, Assoc., Inc. All Rights Reserved.
Privacy Policy | Terms & Conditions
Web Design by CP Solutions.
Marketed by VMD Services.
